The Importance of a Multidisciplinary Approach
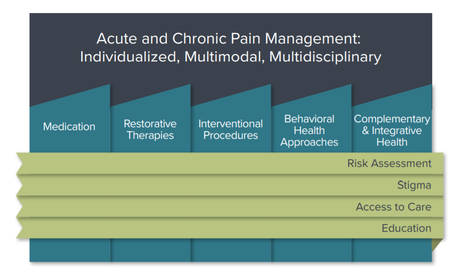 Acute and Chronic Pain Management Consists of Five
Treatment Approaches Informed by Four Critical Topics
Acute and Chronic Pain Management Consists of Five
Treatment Approaches Informed by Four Critical Topics
A multidisciplinary approach for chronic pain across various disciplines, using one or more treatment modalities, is encouraged when clinically indicated to improve outcomes. These include the following five broad treatment categories:
- Medications: Various classes of medications, including non-opioids and opioids, should be considered for use. The choice of medication should be based on the pain diagnosis, the mechanisms of pain, and related co-morbidities following a thorough history, physical exam, other relevant diagnostic procedures and a risk-benefit assessment that demonstrates that the benefits of a medication outweigh the risks.
- Restorative Therapies, including those implemented by physical therapists and occupational therapists (e.g., physiotherapy, therapeutic exercise, and other movement modalities) are valuable components of multidisciplinary, multimodal acute and chronic pain care.
- Interventional Approaches, including image-guided and minimally invasive procedures, are available as diagnostic and therapeutic treatment modalities for acute, acute on chronic, and chronic pain when clinically indicated.
- Behavioral Approaches for psychological, cognitive, emotional, behavioral, and social aspects of pain can have a significant impact on treatment outcomes. Patients with pain and behavioral health comorbidities face challenges that can exacerbate painful conditions as well as function, QOL, and ADLs.
- Complementary and Integrative Health, including treatment modalities such as acupuncture, massage, movement therapies (e.g., yoga, tai chi), and spirituality, should be considered when clinically indicated.
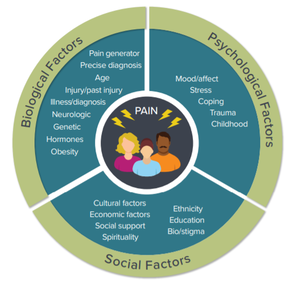
An Individualized, Patient-Centered, and 360° View of Pain Management
|
- Stigma can be a barrier to treatment of painful conditions. Compassionate, empathetic care centered on a patient-clinician relationship is necessary to counter the suffering of patients with painful conditions and to address the various challenges associated with the stigma of living with pain. Stigma often presents a barrier to care and is often cited as a challenge for patients, families, caregivers, and providers.
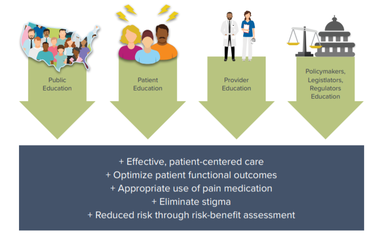 Education Is Critical to the Delivery of Patient-Centered Care
Education Is Critical to the Delivery of Patient-Centered Care
- Improving education about pain conditions and their treatment for patients, families, caregivers, clinicians, and policymakers is vital to enhancing pain care. Patient education can be emphasized through various means, including clinician discussion, informational materials, and web resources. More effective education and training about acute and chronic pain should occur at all levels of clinician training, including undergraduate curricula, graduate training, and continuing professional education. Education for the public as well as for policymakers is emphasized to ensure that expert and cutting-edge understanding incorporated in policy that can affect clinical care and outcomes.
- Addressing barriers to access to care is essential in optimizing pain care. Recommendations include addressing the gap in our workforce for all disciplines involved in pain management. In addition, improved insurance coverage and payment for different pain management modalities is critical to improving access to effective clinical care and should include coverage and payment for care coordination, complex opioid management, and telemedicine. It is also important to note that in many parts of the country, patients have access only to a primary care provider (PCP). Support for education, time, and financial resources for PCPs is essential to managing patients who have painful conditions.
Addressing the Unique Qualities Across All Special Populations
|
Advancing Research and Development
|
2016 CDC Guidelines for Prescribing Opioids for Chronic Pain
- A review of the CDC Guideline (as mandated by the Comprehensive Addiction and Recovery Act legislation):
The Task Force recognizes the utility of the 2016 Guideline for Prescribing Opioids for Chronic Pain released by the CDC and its contribution to mitigating unnecessary opioid exposure and the adverse outcomes associated with opioids. It also recognizes unintended consequences that have resulted following the release of the guidelines in 2016, which are due in part to misapplication or misinterpretation of the guideline, including forced tapers and patient abandonment. - The CDC recently published a pivotal article in the New England Journal of Medicine on April 24, 2019, specifically reiterating that the CDC Guideline has been, in some instances, misinterpreted or misapplied. The authors highlight that the guideline does not address or suggest discontinuation of opioids prescribed at higher dosages. They note, “policies invoking the opioid-prescribing guideline that do not actually reflect its content and nuances can be used to justify actions contrary to the guideline’s intent.” Educating stakeholders about the intent of the guideline (as it relates to the use of opioids for chronic pain by primary care clinicians), re-emphasis of the core benefits of the guideline, and encouraging optimal application of this guideline are essential to optimizing acute and chronic pain care.